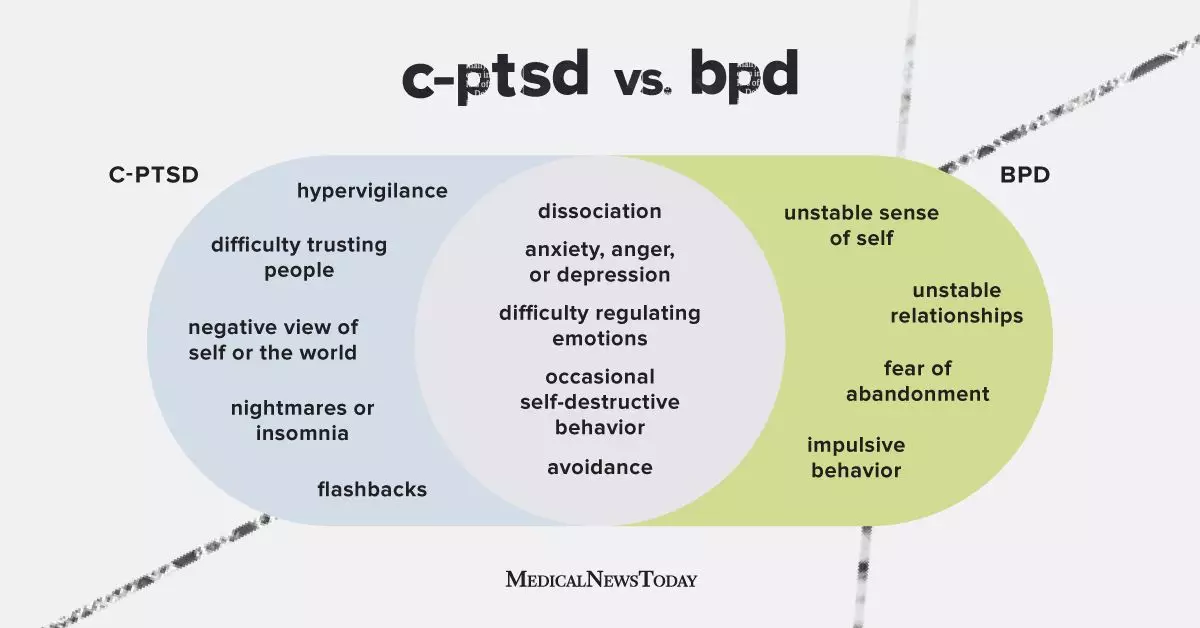
Complex post-traumatic stress disorder (C-PTSD) and borderline personality disorder (BPD) are two mental health conditions that can have overlapping symptoms. While both conditions may lead to feelings of anxiety, depression, anger, or emptiness, they are distinct in their origins and manifestations. C-PTSD typically arises from multiple or ongoing traumatic experiences that a person feels unable to escape, leading to a disrupted sense of safety and a skewed worldview. On the other hand, BPD is a personality disorder characterized by unstable self-image, relationships, and emotions, often causing extreme behaviors and perceptions.
The symptoms of C-PTSD are similar to those of PTSD and may include nightmares, flashbacks, trust issues, negative self-image, and difficulty regulating emotions. In contrast, individuals with BPD may experience unstable relationships, an unclear self-image, emptiness, and intense fluctuations in how they perceive others. While both conditions can result from traumatic experiences, the nature of the symptoms and their impact on daily life can help differentiate between C-PTSD and BPD.
It is important to note that individuals can be diagnosed with both C-PTSD and BPD, as the two conditions may coexist. However, due to symptom overlap and the complexity of trauma-related disorders, there is a risk of misdiagnosis. Factors such as lack of awareness, gaps in memory, and comorbid conditions can contribute to confusion in distinguishing between C-PTSD and BPD. Seeking a comprehensive evaluation by a mental health professional is crucial for accurate diagnosis and appropriate treatment.
Trauma-focused therapy is a primary treatment approach for C-PTSD, aimed at addressing the impact of traumatic experiences on an individual’s daily functioning. Various forms of talk therapy, such as cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), are commonly used to treat BPD, focusing on emotional regulation and relationship skills. While medication may be prescribed to manage specific symptoms, therapy remains a cornerstone of treatment for both C-PTSD and BPD.
Persistent emotional distress, intrusive thoughts, or difficulties in managing symptoms should prompt individuals to seek help from a mental health professional. Open communication and a collaborative approach to treatment can facilitate recovery and improve mental well-being. Whether facing C-PTSD, BPD, or a combination of both, reaching out for support is a vital step towards healing and growth.
Understanding the nuances of C-PTSD and BPD, recognizing their distinct symptoms and treatment options, and seeking appropriate care are essential in navigating these complex mental health conditions. By shedding light on the differences between C-PTSD and BPD, we can empower individuals to advocate for their mental health needs and embark on a journey towards healing and resilience.

Leave a Reply