Pancreatic cancer, a formidable adversary in the realm of oncological diseases, is categorized into four distinct stages, with Stage 2 presenting a critical juncture in the disease’s trajectory. This stage is further divided into Stage 2A and Stage 2B. Stage 2A occurs when the primary tumor exceeds 4 centimeters in diameter, remaining localized within the pancreas. In contrast, Stage 2B is characterized by the tumor potentially varying in size yet having metastasized to a maximum of three neighboring lymph nodes. Understanding the nuances of these stages is essential for both medical professionals and patients alike as they navigate treatment pathways.
Stage 2 pancreatic cancer may initially go undetected due to its subtle onset. By this stage, the cancer is often advanced enough that symptoms start manifesting more prominently. Patients may experience jaundice, indicated by a yellowing of the skin and eyes, along with fatigue that is often debilitating. Unexplained weight loss can occur, suggesting a profound impact on the body’s metabolic processes. Other symptoms might include nausea, vomiting, abdominal pain, and discomfort radiating to the back. Recognizing these signs is vital for timely intervention and management of the disease.
While the precise etiology of pancreatic cancer remains a subject of ongoing research, certain risk factors have been identified. A significant contributor is smoking, which accounts for approximately 20% of pancreatic cancer cases. Additional risk factors include age (with those over 55 being particularly susceptible), obesity, genetic predispositions, and a family history of the disease. Understanding these factors can aid in both prevention strategies and early detection efforts, allowing individuals at higher risk to pursue regular screening.
Diagnosing Stage 2 pancreatic cancer involves a series of comprehensive tests. Healthcare professionals typically utilize imaging technologies such as MRI, CT, or ultrasound scans, which provide insights into the tumor’s size and location. Positron Emission Tomography (PET) scans can help detect cancer cells and evaluate their spread throughout the body. A biopsy may be performed to analyze tumor and tissue samples, confirming cancer presence and progression. Lastly, tumor marker tests are conducted to gauge the growth rate of the malignancy, an essential factor in determining the appropriate treatment plan.
Treatment for Stage 2 pancreatic cancer is multifaceted and often tailored to the individual patient. Surgical options are dependent on whether the cancer is deemed resectable or borderline resectable. A resectable tumor indicates that surgery can typically remove it without significant invasion into surrounding tissues, while borderline cases may necessitate neoadjuvant chemotherapy to shrink the tumor before surgical intervention. The Whipple procedure is a common surgical technique, which entails removing part of the pancreas and adjacent structures, while other procedures may involve total or distal pancreatectomy depending on tumor localization.
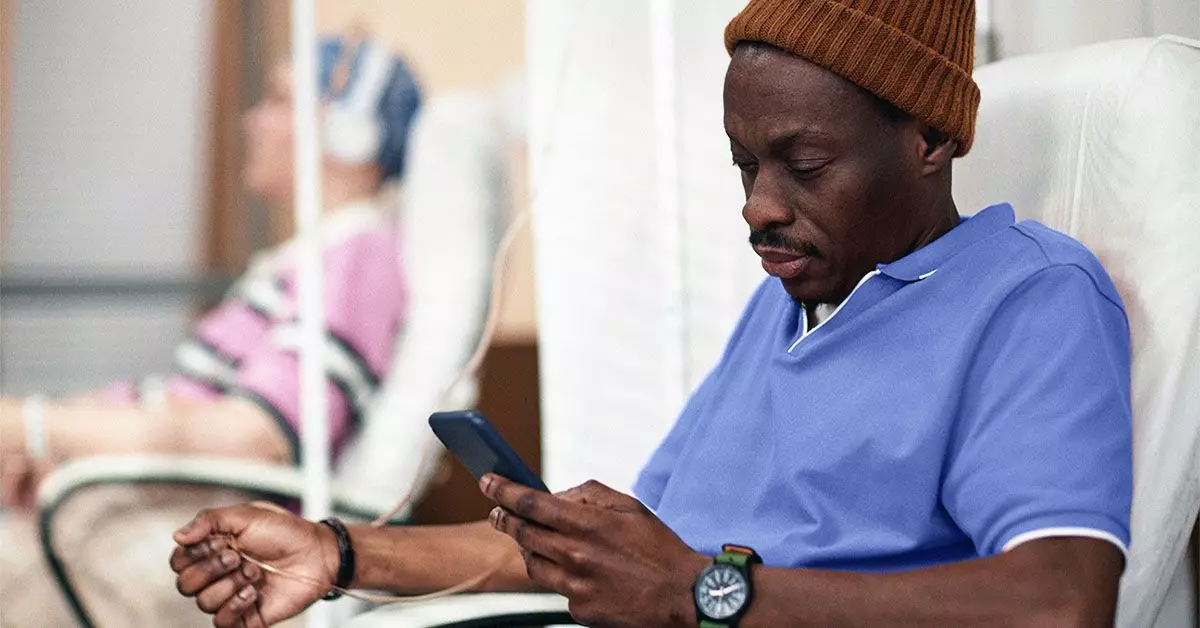
In addition to surgical interventions, chemotherapy is frequently employed as either a primary treatment or as adjuvant therapy following surgery to mitigate recurrence risks. Radiation therapy may also be considered, functioning in tandem with other treatments to optimize patient outcomes. The comprehensive approach combining these modalities aims to extend survival and improve quality of life.
While Stage 2 pancreatic cancer is classified as less severe than later stages, its prognosis remains challenging. The five-year survival rate for this diagnosis ranges from 5% to 15%, reflecting the aggressive nature of this malignancy. Individual outcomes can vary based on numerous factors, including tumor size, location, resectability, and overall patient health. It is crucial for patients and their families to engage in open conversations with their healthcare providers to grasp the implications of their unique circumstances and treatment options.
Stage 2 pancreatic cancer represents a significant challenge in cancer treatment. With its specific sub-stages, treatment possibilities, and distinct symptoms, understanding this disease is essential for effective management and intervention. Patients diagnosed with Stage 2 pancreatic cancer should seek comprehensive care that evaluates all potential treatment options, keeping in mind the complexities of this multifaceted illness. Continuous research and advancements in medical science hold promise for improving outcomes and survival rates for future patients battling pancreatic cancer.

Leave a Reply