Cancer treatments such as radiotherapy, chemotherapy, and surgery have been known to have various side effects on the human body. One of the common side effects includes damaging the thyroid and leading to hypothyroidism. Hypothyroidism is a condition where the thyroid gland fails to produce enough hormones to carry out its normal functions. Given that the thyroid plays a critical role in energy regulation, any damage to this gland can have a significant impact on overall health.
Various cancer treatments can increase the risk of hypothyroidism in different ways. For example, surgical procedures or radiation therapy can directly damage or remove thyroid tissue, leading to a decrease in thyroid hormone production. Similarly, certain chemotherapy drugs or medications can interfere with thyroid hormone production or trigger autoimmune responses that attack the thyroid. Interestingly, a study from 2020 found that the risk of hypothyroidism was higher in individuals who had undergone treatment for breast cancer, regardless of the type of treatment received.
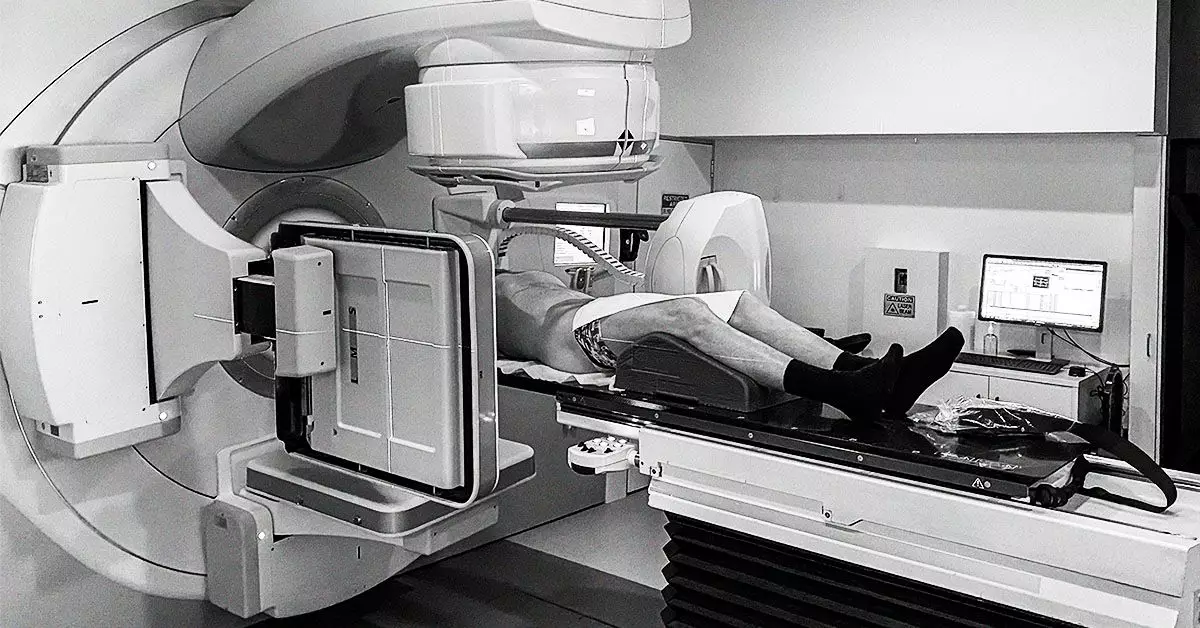
Impact of Radiation Therapy on Thyroid Health
According to recent reviews, radiation therapy for head and neck cancers can pose a significant risk of hypothyroidism. In some cases, up to 40-50% of individuals who receive radiation therapy may develop hypothyroidism due to the susceptibility of the thyroid gland to radiation. Factors such as the radiation dose, type of therapy, original thyroid size, sex, and age can all influence the likelihood of developing hypothyroidism.
Thyroid Health and Surgical Interventions
Surgery to remove cancerous thyroid tissue is a common treatment for thyroid cancer. However, depending on the extent of the cancer, partial or total removal of the thyroid gland may be necessary. As a result, the thyroid’s ability to produce hormones is compromised, leading to the development of hypothyroidism. Hormone therapy medications designed to block thyroid-stimulating hormone (TSH) can also induce hypothyroidism in some cases to prevent the recurrence of thyroid cancer.
Immunotherapy involving immune checkpoint inhibitors can target cancer cells effectively but may also cause inflammation of the thyroid gland. Specific proteins known as antithyroid antibodies can trigger this inflammation, leading to thyroid dysfunction. While some individuals may experience increased thyroid activity initially, hypothyroidism may develop over time. Interestingly, those who developed thyroid problems during treatment had higher cancer survival rates a year after treatment.
Management of Hypothyroidism in Cancer Survivors
For individuals who develop hypothyroidism as a result of cancer treatment, lifelong thyroid hormone replacement therapy may be necessary. Levothyroxine, a synthetic form of thyroid hormone, can help regulate energy metabolism and minimize the risk of thyroid cancer recurrence. Additionally, certain types of cancer, such as pituitary tumors or papillary thyroid cancer, may have direct implications for thyroid health and hormone production.
It is crucial for healthcare providers and cancer survivors to be aware of the potential impact of cancer treatments on thyroid health. Monitoring thyroid function and initiating appropriate interventions can help mitigate the risk of hypothyroidism and its associated complications in cancer survivors. Through a comprehensive understanding of these interactions, healthcare professionals can optimize the long-term health outcomes of individuals undergoing cancer treatment.

Leave a Reply